111 | Sample Sizes for Food Testing | New Food Bacteria Linked to Mystery Illnesses | BPA Toxicity |
Plus a warning about pumpkins
This is The Rotten Apple, an inside view of food integrity for professionals, policy-makers and purveyors. Subscribe for weekly insights, latest news and emerging trends in food safety, food authenticity and sustainable supply chains.
Sample sizes for food safety tests;
Packaging chemicals safety - new information;
An underestimated (new) food pathogen (Helicobacter pullorum) - does it cause Crohn’s disease?
Food safety news and resources from around the globe;
A big knife is still a big knife (just for fun);
Food fraud news, emerging issues and recent incidents
🎧 Listen Now (for paying subscribers) 🎧
Welcome to another week of food safety/fraud goodness.
Thank you for trusting me with your time and making space in your inbox for me each week. I love you all*!
This week’s hero story was supposed to be a nerdy exploration of the statistics of sample sizes for food testing. But I’m actually more excited by the story about a new(ish) food-borne bacterium Helicobacter pullorum, which has been linked to long-term gastric illnesses including Crohn’s disease. I hope you find it as intriguing as I did while researching it.
Also this week, BPA safety is in the spotlight (again!), plus a new food fraud trend in Europe with millions of food packs affected.
And 🎃pumpkins.
Karen
P.S. *I especially love those of you who support my work financially 👏 Huge shoutout to Uma from Canada for signing up. And to Laurie, Brian, Sandra, Tshane and Michael for your ongoing support 👏 I couldn’t do this without you. Thank you ♥
Sample Sizes for Food Safety Tests
What size sample should you take when testing a batch or lot of food? It’s a tricky question.
Large sample sizes produce a more precise estimate of the food but are more costly to collect and test. Smaller sample sizes are less reliable but more cost-effective. Therefore, an appropriate sample size needs to be calculated using good science.
Researchers have published a new paper about statistically reliable sample sizes for food safety tests. Spoiler alert: for detecting microbial contamination, sample sizes need to be large.
Terminology note: In this article, a sample is the quantity of food that will be tested and that is supposed to represent the lot or batch of food. The sample is made up of a series of units selected from the lot. A unit is a single portion of the lot, such as a pot of yoghurt, five lettuces, 2 kg of grain, or 4L of milk. Sample size is the number of units in the sample.
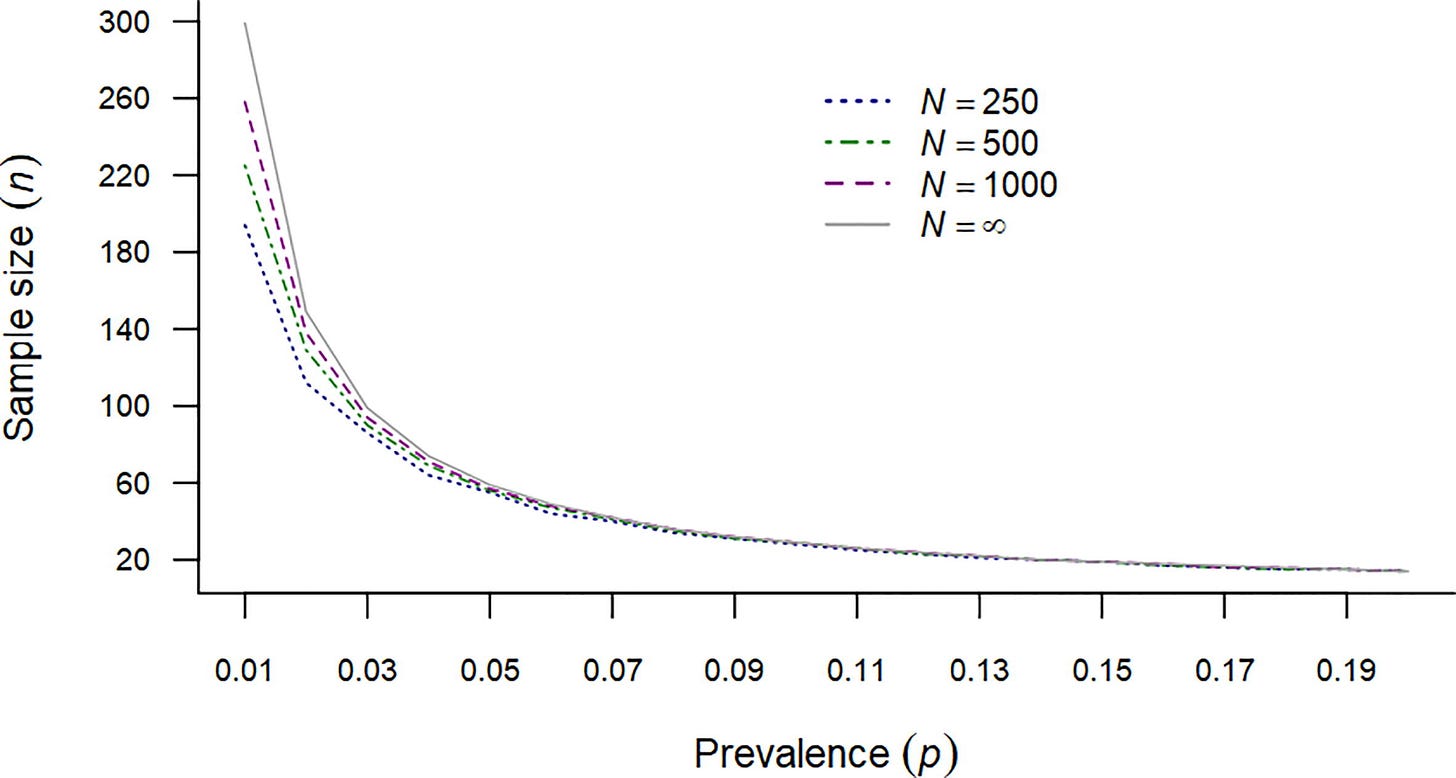
The results of their work might be surprising for some readers. For example, if Listeria monocytogenes is present in 1% of packages of food from a single batch, you would have to test 299 packages to have a 95% chance of finding it, assuming the number of packages in the batch of food is greater than 4,000.
If the lot size is small, for example, 250 packages of pre-cut cantaloupe (rock melon), you would need to test 194 packages to be sure of finding L. monocytogenes if it is present in 1% of the packages. Yes, 194 out of 250 packs. That would mean testing more than three-quarters of the packs in the batch!
On the other hand, if the contamination is more pervasive… say, if L. monocytogenes was present in 4% of packs, instead of 1%, you would need to test around one-quarter of packs to be sure of finding it – or (more correctly) to have a 95% chance of finding it.
Similarly, researchers estimated that with the estimated prevalence of Salmonella enteritidis in US eggs at 1 in 20,000 eggs, you would need to test almost 60,000 eggs to have a 95% chance of detecting Salmonella.
I hardly need to tell you that testing sixty thousand samples of food to detect a pathogen is infeasible.
How statisticians handle the sample size challenge
The alternative to testing such a high proportion of samples is to instead use a method that estimates maximum prevalence; that is, an estimate of whether the number of contaminated units in a batch/lot exceeds a certain threshold. Sampling programs that use this method are called acceptance plans. In food sampling, the threshold is often zero.
The calculations for this method, with a zero acceptance level, look like this:
In this formula (‘inequality’), the left side represents the probability of getting at least one contaminated unit in the sample and the right side is the probability of not finding a contaminated sample. N is the number of units in the lot or batch, n is the number of units to be tested, K is the number of contaminated units in the batch and P<0> is the probability of not finding any contaminated units.
The minimum sample size is the smallest value of n that satisfies the inequality.
For example, if a public health agency wanted to test a batch of eggs for Salmonella enteritidis while investigating a foodborne illness outbreak, and if there are currently 75,000 unsold eggs from the batch, and if ‘normal’ contamination rates are known to be 1 in 20,000, they could choose an acceptance level of, say, 1 in 10,000.
This would give a K threshold of 75000 x (1/10,000) = 7.5. When these numbers are used in the formula above, for a 90% confidence level, the number of eggs that would need to be tested would be 21,000. And the probability of having no more than one contaminated egg out of every 10,000 eggs in the batch is 90% if none of the eggs in the sample tested positive.
To reduce the number of samples that would have to be tested in this scenario, the agency would need to select either a higher acceptable contamination rate (say 1 in 2,500 eggs) or use a lower confidence level.
Takeaways for food professionals
Finding contaminants that are present at low levels in a batch of food is statistically difficult, and requires a very large proportion of units of food to be tested, if precise results are needed. Testing fewer units gives results with a lower confidence level – that is, results that are less likely to be ‘true’.
There are software packages and publicly available methods to calculate sample sizes for food testing, including those published by the International Organization for Standardization (ISO) and the Codex Alimentarius Commission (CAC),.
Learn more:
Statistical aspects of microbiological criteria related to foods: a risk managers guide (FAO, 2016)
Codex Alimentarius Commission (CAC). (2004). CAC/GL 50-2004: General guidelines on sampling. Codex Alimentarius Commission
Source: Wang, S.S., Canida, T.A., Ihrie, J.D. and Chirtel, S.J. (2023). Sample Size Determination for Food Sampling. Journal of Food Protection, [online] 86(9), p.100134. doi: https://doi.org/10.1016/j.jfp.2023.100134
How BPA and DEHP in food packaging cause health problems – autism link found
Bisphenol A (BPA), and Diethylhexyl Phthalate (DEHP), chemical additives used in some types of food packaging including polycarbonate beverage bottles and linings for metal food and beverage cans, and in baby bottles, have long been accused of damaging our health.
Earlier this year, the European Union’s Food Safety Authority (EFSA) reassessed safety limits for BPA and decided they were too high. By a factor of ten thousand! They recommended that BPA safety limits be reduced from an intake of 4 micrograms per kilogram of body weight per day to 0.2 nanograms. They also found that many consumers would be exceeding the new daily intake guidance.
Past studies have shown possible health risks from BPA and DEHP, including one that observed links between exposure to environmental pollutants such as BPA and DEHP and autism however the reason for the links has not been clear.
New research, however, might explain how these chemicals could be linked to behavioural problems such as autism and ADHD in children.
Results from a new US study suggest that some children are less able to excrete BPA and DEHP from their bodies than others. The study examined 149 children between 3 and 16 years of age, including children with autism, ADHD and neurotypical children.
Children from the three groups were found to have different metabolic pathways for excreting BPA and DEHP but were otherwise similar with respect to their metabolic pathways. Neurotypical children were significantly more efficient at excreting BPA via a pathway known as glucuronidation than children with autism or ADHD. The same trends were observed for DEHP excretion but were not statistically significant.
Source: Stein TP, Schluter MD, Steer RA, Ming X (2023) Bisphenol-A and phthalate metabolism in children with neurodevelopmental disorders. PLoS ONE 18(9): e0289841. https://doi.org/10.1371/journal.pone.0289841
Does this newly discovered bacterium cause chronic gastric diseases like Crohns?
Helicobacter pullorum - an emerging (underestimated) food safety risk
In 2005 two researchers were awarded the Nobel prize for busting the long-held belief that gastric ulcers (stomach ulcers) were caused by stress. They proved that ulcers were not caused by stress but by the actions of a bacterium that can survive inside human stomachs and grow to damage the stomach lining. The bacteria was Helicobacter pylori.
Now, microbiologists are asking whether H. pylori’s ‘cousin’, Helicobacter pullorum, could also be causing havoc in our guts.
Fun fact: the medical community was so dismissive of the bacterial theory of gastric ulcers that one of the researchers deliberately infected himself with Helicobacter pylori by drinking a beakerful of H. pylori-filled broth to prove his theory. He got very sick before curing himself with antibiotics. He and his colleague were awarded the Nobel prize 20 years later.
Helicobacter pullorum, from the same genus as the gastric ulcer bacterium, is a newly categorised (1994) bacterial species which has been linked to chronic gastrointestinal illnesses such as Chron’s disease and gall bladder malignancies. It is found in the gastrointestinal tract of poultry birds and in their meat.

H. pullorum has characteristics which allow it to survive gastric “stresses” such as bile acids, similar to Campylobacter jejuni (a foodborne pathogen) and Helicobacter pylori.
It causes gastroenteritis in domesticated chickens, turkeys, and guinea fowl. In humans, it has been found in people with chronic bowel conditions including Crohn's disease, cholelithiasis and gall bladder malignancies, but less commonly in healthy individuals.
In some countries, it can be found in a high proportion of poultry birds. For example, in Italy it was found in 100% of chickens from broiler farms, while in Malaysia it has been found in 25% of broiler and village chickens.
Helicobacter pullorum can be transmitted to humans through contaminated meat, posing food safety risks. Despite the high prevalence of H. pullorum in poultry, and its potential links to serious long-term illness, this bacterium, say researchers, has received little attention.
Source: Helicobacter pullorum: An Emerging Zoonotic Pathogen
🍏 Read more: The Remarkable Story of the Unapproved Medical Experiment that ‘Proved’ the Cause of Gastric Ulcers 🍏
Food Safety News and Resources
23 October | Food Safety News and Free Resources | Recall: Frozen burritos for L. monocytogenes (USA) | Recall: Enoki mushrooms for L. monocytogenes (USA) | Chemical residues in food - survey results (Canada) | Food Toxin Risks Ranked (Europe) | Innovation in Allergen Management Information |
A Big Knife is Still a Big Knife on Halloween (Just for fun)
This safety message from the US Product Safety Commission wins my Tweet of the week award (“Awake, cousins, awake, it’s time!”)

What you missed in last week’s email
Emerging Food Safety Risks
Training session replay: Pest Management and the Principles of IPM
Underestimating the Scope of Food Fraud
Why the US Food Industry is Running Scared
Below for paying subscribers: Food fraud news, emerging issues and incident reports
📌 Food Fraud News 📌
New Food Fraud Trend: Fraudulent ‘Recycling’ of Dumped Food on a Massive Scale
Europol’s anti-food fraud operation, Opson XII, conducted between Dec 2022 and April 2023, included a focus on the ‘recycling’ of spoiled or expired food to “reduce production costs” (huh?). Europol reported that “the relatively new trend of relabelling expired food has been detected on an unprecedented scale”.
Changing expiry dates on old food is



