146 | Crisis Plan Resources | Hepatitis E Primer | Fake Mushrooms |
And an in-person meetup next week at IAFP
Meetup (in person!) at IAFP next week;
Crisis Management Resources;
Everything you need to know about hepatitis E;
Food Safety News and Resources;
How to fake a mushroom;
Food fraud news, emerging issues and recent incidents
Hi,
Did you know hepatitis E is one of the top three viral foodborne illnesses, together with hep A and norovirus? Me neither! At least not until I wrote this week’s newsletter.
Welcome to Issue 146 of The Rotten Apple. If you’ve just upgraded to a paid subscription, you got 25% off for life! Congratulations.
This week’s issue features a crisis planning resources supplement for paying subscribers, plus some interesting news about mad cow-like disease (Creutzfeldt-Jakob) surfacing in people who ate venison. Find that in our weekly food safety news roundup.
Our July meetup is in person (exciting) at the annual IAFP conference in California. Details below. I hope to see you there.
Karen
P.S. If you love this newsletter, please tell your friends and colleagues about it and help grow our community of global food safety champions.
Meetup next week at IAFP
I’m excited to be attending the annual conference of the International Association for Food Protection next week in Long Beach, California. If you’ll be there too and would like to meet in person, reply to this email and I’ll send a meeting time poll so we can find a time that works for everyone.
Crisis Management Plans
Food businesses can’t afford to stop making food if something goes wrong. But how to make sure your products and consumers are safe after a disaster? Our supplement for paying subscribers has:
guidance on crisis management procedures;
a complete plan outline;
suggested contact lists and team roles and responsibilities;
example scenarios;
a downloadable crisis management checklist for mock crisis exercises and real crisis events.
Click the link below to view it.
Crisis Management Plans for Food Businesses
Why have a crisis management plan? When a crisis happens, food businesses don’t just stop making and selling food. However, continuing to operate in a crisis can compromise food safety. Effective crisis planning will allow a food business to remain operational and ensure that food can still be produced safely after a crisis.
Everything you need to know about Hepatitis E
Globally, there are around 5 million cases of acute viral hepatitis due to either hepatitis A virus (HAV) or hepatitis E virus (HEV) annually. In the past 20 years cases have soared, increasing tenfold.
Hepatitis E and hepatitis A, together with norovirus, make up the top three causes of viral foodborne illnesses, with hepatitis A and E being considered more clinically severe than norovirus.
Let’s explore how hepatitis E infections can arise from foodstuffs, why it’s such a risk, and what control measures are available.
What is Hepatitis E?
Hepatitis E is a liver disease caused by the hepatitis E virus (HEV). It remains a significant public health concern, particularly in regions with poor sanitation.
The virus is primarily transmitted via the faecal-oral route, often via contaminated water or food. Most commonly, outbreaks are linked to the consumption of undercooked meat or shellfish and drinking water contaminated with faeces.
The disease presents with symptoms such as jaundice, fatigue, nausea, and abdominal pain. In most people, the condition is self-limiting, but it does pose a severe risk to pregnant women, older adults and immunocompromised individuals.
Symptoms begin up to ten weeks after exposure, with the typical infection incubation period being five to six weeks. They can last up to six weeks and include an initial phase with fever, nausea and vomiting, followed by symptoms of liver inflammation including abdominal pain, rashes, jaundice, dark urine and pale stools.
Hepatitis E infection can lead to acute liver failure, especially in pregnant women. Patients who experience liver failure are at risk of death.
Common Food Vectors
Common food vectors for hepatitis E include:
· Pork and Pork Products: HEV is often found in undercooked or raw pork and pork products like liver sausages and pâté. Both wild boar meat and raw venison also carry a significant risk, although pigs remain the primary reservoir for zoonotic HEV.
· Shellfish: Contaminated shellfish, particularly bivalve molluscs such as clams, oysters, and mussels, can carry HEV, when harvested from polluted waters.
· Soft Fruits: Soft fruits, such as berries, can become contaminated with HEV through irrigation with contaminated water or improper handling.
· Contaminated Water: Drinking water contaminated with faeces from infected individuals or animals is a significant vector for HEV.
Soft fruits may seem like a surprising addition to the list. However, a 2023 analysis found that soft fruits are at risk of being contaminated by enteric viruses. After testing berries purchased in Ireland, researchers found evidence of the virus in 6.7% of samples.
Recent cases
In March 2024, Finland recalled meat products from across the country as people fell ill with hepatitis E. Eighty-one cases were identified by the Infectious Disease Register, with half of the victims requiring hospital treatment. The illnesses were linked to salami; several brands recalled their products after the findings.
Confirmed cases of hepatitis E have skyrocketed in Europe in recent years, from around 500 cases in 2005 to more than 5,000 a decade later.

The bulk of European cases were due to zoonotic transmission with pork and wild boar products being the major sources.
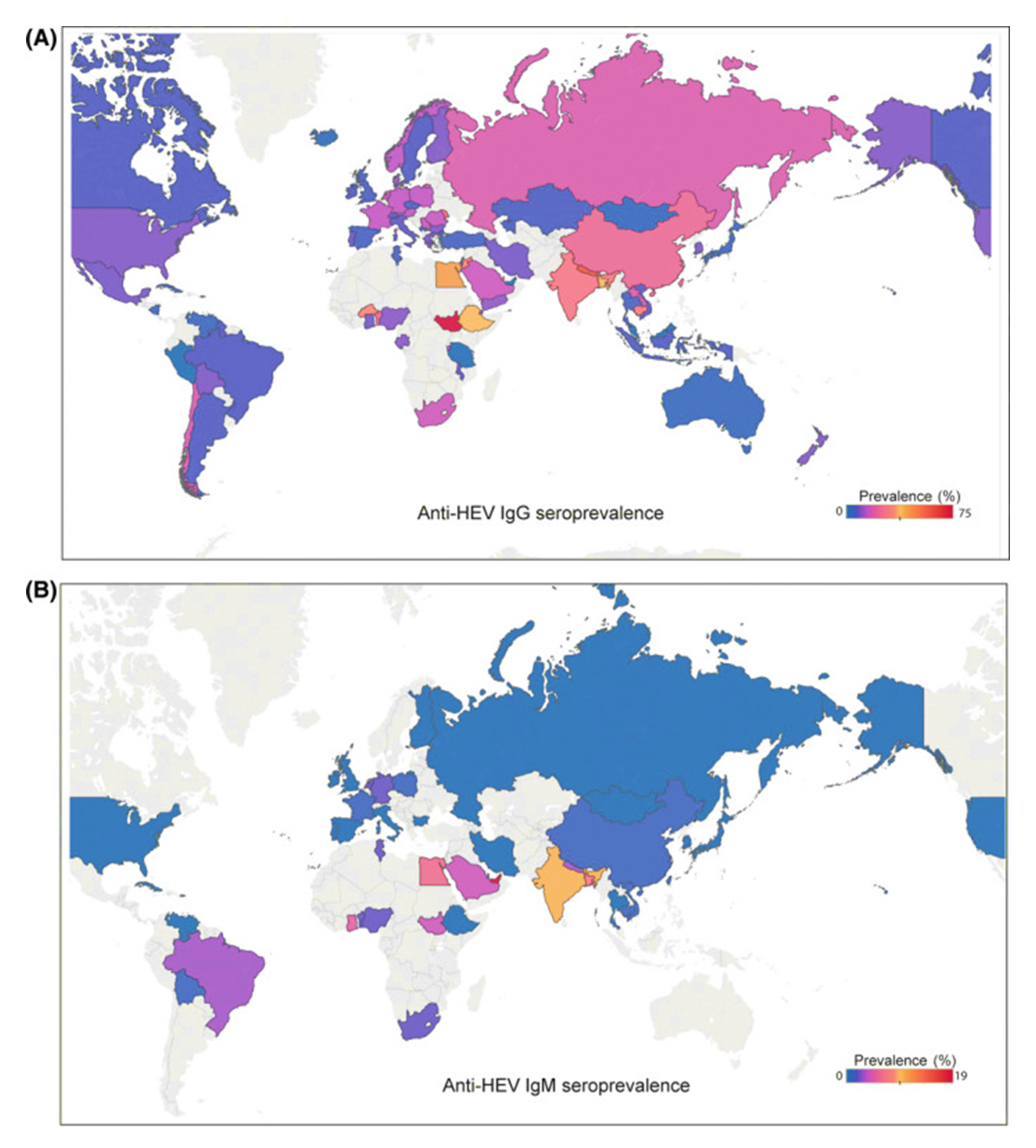
Where Is Hepatitis E Globally?
Not all parts of the world carry the same risk of hepatitis E. The highest numbers of cases occur in places where contaminated water supplies or food sources are most prevalent.
Hepatitis E infection hotspots include:
· South Asia: Countries like India, Nepal, and Bangladesh experience frequent outbreaks due to contaminated water supplies.
· East and Southeast Asia: China, Vietnam, and Myanmar report numerous cases, often linked to consumption of contaminated food and water.
· Africa: Several African countries, including Chad, Sudan, and Nigeria, face regular hepatitis E outbreaks, exacerbated by inadequate sanitation infrastructure.
· Middle East: Nations such as Pakistan and Iran see significant hepatitis E incidence, often related to both food and waterborne transmission.
· Latin America: Areas in Mexico and Bolivia report sporadic outbreaks, usually linked to poor water quality and hygiene practices.
Hepatitis E preventive measures
There is no one-size-fits-all solution to solve foodborne outbreaks of hepatitis E. It requires changes in hygiene standards, food safety, and public health infrastructure.
Key measures include:
1. Sanitation and Water Quality. Access to clean water is fundamental to reducing cases. Not only does that reduce direct consumption, but it also prevents food contamination. Water should be treated to eliminate viral contaminants, and sewage must be disposed of correctly.
2. Food Handling and Preparation. Educating food handlers about safe practices is essential. This includes thorough cooking of meat, particularly pork and shellfish, to kill the virus, and avoiding cross-contamination in kitchens.
3. Surveillance and Monitoring. Local authorities and national health centres should continually monitor for new cases, detecting sources of contamination to prevent spread.
Sources:
WHO (2019). Hepatitis E. [online] Who.int. Available at: https://www.who.int/news-room/fact-sheets/detail/hepatitis-e.
Ricci, A., Allende, A., Bolton, D., Chemaly, M., Davies, R., Fernandez Escamez, P.S., Herman, L., Koutsoumanis, K., Lindqvist, R., Nørrung, B., Robertson, L., Ru, G., Sanaa, M., Simmons, M., Skandamis, P., Snary, E., Speybroeck, N., Ter Kuile, B., Threlfall, J. and Wahlström, H. (2017). Public health risks associated with hepatitis E virus (HEV) as a food‐borne pathogen. EFSA Journal, 15(7). doi: https://doi.org/10.2903/j.efsa.2017.4886.
Li, P., Liu, J., Li, Y., Su, J., Ma, Z., Bramer, W.M., Cao, W., Man, R.A., Peppelenbosch, M.P. and Pan, Q. (2020). The global epidemiology of hepatitis E virus infection: A systematic review and meta‐analysis. Liver International, 40(7), pp.1516–1528. doi: https://doi.org/10.1111/liv.14468.
Ricci, A., Allende, A., Bolton, D., Chemaly, M., Davies, R., Fernandez Escamez, P.S., Herman, L., Koutsoumanis, K., Lindqvist, R., Nørrung, B., Robertson, L., Ru, G., Sanaa, M., Simmons, M., Skandamis, P., Snary, E., Speybroeck, N., Ter Kuile, B., Threlfall, J. and Wahlström, H. (2017). Public health risks associated with hepatitis E virus (HEV) as a food‐borne pathogen. EFSA Journal, 15(7). doi: https://doi.org/10.2903/j.efsa.2017.4886.
Further reading:
Food Safety News and Resources
My weekly food safety news roundups are free for everyone. Click the preview below to read.
This week’s highlights:
Prion disease (like Mad Cow Disease) kills men who ate deer infected with (deer) chronic wasting disease.
Bread manufacturer warned for declaring allergens as ingredients (USA).
Food Safety News and Resources | July
8 July | Food Safety News and Free Resources | Deaths from Creutzfeldt-Jakob disease (USA) | Mushroom gummies recalled after consumers hospitalized (Australia) | Microplastics in edible oil | Salmonella in cucumbers: source found (USA) | Bread manufacturer warned for declaring allergens (USA) |
How to Fake a Mushroom (Just for Fun)
Artist Kerry Samantha Boyes makes fake food for Hollywood. Here’s how she makes mushrooms.
Below for paying subscribers: Food fraud news, research and incident reports
📌 Food Fraud News 📌
In this week’s food fraud news:
📌 Report: Intentional Adulteration of Foods with Chemicals;
📌 Suspected Frauds in Europe (Agri-food and Feed Latest Report);
📌 Milk, fish warnings.
📌 Suspicious mushrooms.






